Human Immunodeficiency Virus (HIV) remains one of the world's most challenging public health issues, affecting over 38 million people globally. While no cure exists yet, the development and widespread use of anti-retroviral drugs (ARVs) have transformed HIV from a fatal diagnosis into a manageable chronic condition for millions. Therefore, in this blog, we will delve into what anti-retroviral drugs are, how they work, the different classes, their side effects, and their broader impact on global health.
What is the Treatment for HIV?
The treatment for HIV is called antiretroviral therapy (ART). In essence, ART involves taking a combination of HIV medicines (called an HIV treatment regimen) on a regular schedule, usually every day (pills) or once a month/every two months (injections). In fact, it is recommended for everyone who has HIV. Although ART cannot cure HIV, these HIV medicines help people with HIV live long, healthy lives. Furthermore, ART also reduces the risk of HIV transmission.How Do HIV Medicines Work?
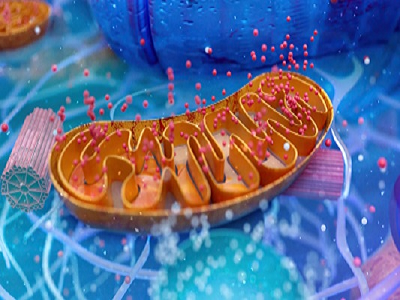
HIV attacks and destroys the infection-fighting CD4 T lymphocytes (CD4 cells) of the immune system. As a result, the loss of CD4 cells makes it hard for the body to fight off infections, including opportunistic infections and some HIV-related cancers. Fortunately, HIV medicines prevent HIV from multiplying (making copies of itself), which reduces the amount of HIV in the body (called the viral load). Consequently, having less HIV in the body gives the immune system a chance to recover and produce more infection-fighting CD4 cells. Even though there may still be HIV in the body, the additional CD4 cells keep the immune system strong enough to fight off infections. Additionally, by reducing the amount of HIV in the body, HIV medicines also reduce the risk of HIV transmission. One of the main goals of HIV treatment, therefore, is to reduce a person's viral load to an undetectable level. This is crucial because people with HIV who maintain an undetectable viral load have effectively no risk of transmitting HIV through sex, and a significantly lower risk of transmission through other means (such as shared needles).Objectives
- To begin with, identify the mechanism of action of HIV medications approved by the Food and Drug Administration.
- Next, identify the adverse effects of HIV antiretroviral therapy medications.
- In addition, determine the appropriate monitoring steps for antiretroviral therapy medications.
- Finally, communicate the importance of improving care coordination amongst the interprofessional team to enhance care delivery for patients with HIV and improve outcomes.
Types of Antiretroviral Medications
There are six main types (?classes') of antiretroviral drugs. Each class works at a different stage of the HIV lifecycle to stop it from making new viruses. Generally, drugs from two (or sometimes three) classes are combined to ensure a combined attack on HIV. The four main classes, which are the basis for most treatments, target one of three viral proteins that control HIV's lifecycle: reverse transcriptase, integrase, and protease.-
Nucleoside/Nucleotide Reverse Transcriptase Inhibitors (NRTIs)
- Abacavir
- Emtricitabine
- Lamivudine
- Tenofovir disoproxil
- Tenofovir alafenamide
- Zidovudine
-
Non-nucleoside Reverse Transcriptase Inhibitors (NNRTIs)
- Doravirine
- Efavirenz
- Etravirine
- Nevirapine
- Rilpivirine
-
Integrase Inhibitors
- Biktarvy
- Dolutegravir
- Elvitegravir
- Raltegravir
- Vocabria
-
Protease Inhibitors (PIs)
- Atazanavir
- Darunavir
- Lopinavir
-
Booster Drugs
- Ritonavir
- Cobicistat
Key Developments in Anti-Retroviral Therapy
- According to ViiV Healthcare data, 89% of treatment-naïve people with HIV on July 14, 2025, opted to switch to long-acting injectable Vocabria + Rekambys following rapid viral suppression with daily Dovato.
- Similarly, Merck announced the initiation of the EXPrESSIVE Phase 3 clinical trials, evaluating the safety and efficacy of MK-8527, an investigational once-monthly oral nucleoside reverse transcriptase translocation inhibitor (NRTTI) for HIV pre-exposure prophylaxis (PrEP).
- Furthermore, the U.S. FDA accepted a New Drug Application for Merck's Doravirine/Islatravir, an investigational once-daily, oral, two-drug regimen for the treatment of adults with virologically suppressed HIV-1 infection.