High blood pressure, medically known as hypertension, is a powerful and silent threat to your kidneys that quietly causes damage long before symptoms appear. In fact, persistently elevated blood pressure levels gradually weaken and injure delicate blood vessels, making the kidneys less able to filter blood efficiently and maintain fluid balance. This unseen harm often continues for years, and only becomes noticeable once serious kidney damage has already occurred.
First, let’s understand what high blood pressure really means. As your heart beats, it pumps blood into your arteries, which creates pressure from the blood pushed against their walls. When the pressure in your arteries rises above normal levels (more than 130/80 mmHg), your heart works harder than usual to pump blood through the vascular system. This extra effort over time causes injury not only to the heart but to many other vessels in the body, including both your kidneys' blood supply.
Your kidneys, located on either side of your spine, act like sophisticated filtering machines. Every minute, they filter about half a cup of blood, removing waste products, excess water, and balancing electrolytes to maintain internal harmony. They also help regulate blood pressure by releasing hormones that signal blood vessel constriction and fluid balance.
The Silent Damage Begins
Initially, high blood pressure may not show any obvious symptoms. Therefore, both high blood pressure and damage to the kidneys early on can be categorized as ""silent."" This means that most people will feel fine even when their blood vessels are slowly deteriorating. When you do not check your blood pressure regularly or test how well your kidneys work, kidney and blood vessel damage can continue for many years without your awareness.
Here’s how the silent destruction unfolds:
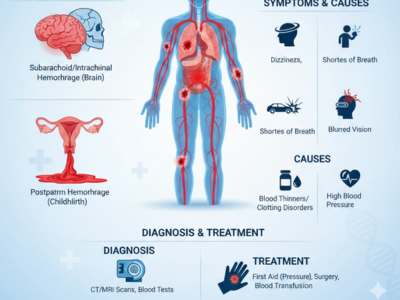
- Blood Vessel Damage: The small and delicate blood vessels located in the kidneys receive constant pressure from the blood flow that runs through them as a result of elevated blood pressure. As time passed by, the mechanical pressure exerted on these vessels caused them to narrow, harden, or develop stiffness (arteriosclerosis). As these vessels deteriorate, less blood can reach the filtration structures of the kidneys.
- Reduced Filtration: Inside each kidney, thousands of microscopic filters called nephrons actively clean the blood. When reduced blood flow damages blood vessel walls, these nephrons work less effectively. As a result, waste products and excess fluid build up in the body instead of being eliminated.
- Scar Formation: Continuous pressure and damaged blood flow lead to scarring within the kidney tissue. This scarring permanently reduces the organ’s ability to filter blood, and each damaged nephron further weakens kidney function.
- Dangerous Feedback Loop: Damaged kidneys struggle to regulate blood pressure. As a result, they may retain excess fluid and salt, which increases blood volume and further raises blood pressure. This vicious cycle accelerates both hypertension and kidney damage, making each condition worse than before.
Why Early Stages Go Unnoticed
The problem with kidney damage from high blood pressure is that there are no symptoms in the early stages. This is why some people do not know they have a problem until their kidneys are badly damaged. Some people may experience symptoms when their kidneys are badly damaged. These symptoms may include swelling in the feet and ankles, fatigue, loss of appetite, stomach upset, changes in urination, and difficulty concentrating.
Regular health check-ups are a must, especially for people who have risk factors such as age, family history of high blood pressure, diabetes, and an unhealthy lifestyle. Early detection of high blood pressure and kidney damage can help prevent permanent damage to the kidneys.
The number of people diagnosed with diabetes is constantly increasing due to lifestyle changes, sedentary living, unhealthy eating habits, and obesity gaining ground; the need for trustworthy glucose monitoring tools is growing continuously. Major health care providers, insurance companies, and drug manufacturers highlight the need for early detection and ongoing monitoring to minimize diabetes-related complications such as heart disease, kidney problems, and nerve damage.
How High Blood Pressure and Kidney Disease Feed Each Other
High blood pressure and kidney disease have a bidirectional relationship. This means that not only can hypertension cause kidney damage, but impaired kidneys can also contribute to worsening high blood pressure. The kidneys play a key role in managing blood volume and hormone release that affects blood pressure. When these functions are compromised, the body loses vital blood pressure control mechanisms.
This creates a harmful feedback loop:
- Elevated blood pressure damages the kidney’s blood vessels.
- Weakened kidneys fail to manage blood pressure effectively.
- Increasing blood pressure causes further kidney damage.
Who Is at Risk?
Anyone can develop high blood pressure, but certain factors raise the chances significantly. These include:
- Age: Blood pressure tends to rise with age.
- Genetics: A family history of hypertension increases your risk.
- Lifestyle Habits: High salt intake, sedentary behavior, smoking, and excessive alcohol use can elevate blood pressure.
- Other Conditions: Diabetes and high cholesterol often occur alongside hypertension and compound the risk for kidney damage.
It’s important to recognize these risk factors early, as they are often modifiable. With appropriate lifestyle changes and medical support, you can drastically lower your chances of developing serious complications.
Prevention and Protection: What You Can Do
While high blood pressure and kidney damage might be silent, you can take steps to protect your health and reduce your risk:
- Monitor Regularly: Get your blood pressure checked frequently, especially if you are over 40 or have risk factors. Know your numbers and track changes over time.
- Stay Physically Active: Regular exercise helps keep blood pressure within a healthy range and supports weight management.
- Adopt a Kidney-Friendly Diet: Reduce sodium intake, eat plenty of fruits and vegetables, and choose whole grains and lean proteins. A balanced diet can lower blood pressure and support overall health.
- Manage Weight: Maintaining a healthy weight reduces the strain on your cardiovascular system and kidneys.
- Avoid Smoking and Excess Alcohol: These habits directly harm your blood vessels and support pathways that raise blood pressure.
- Consult Healthcare Providers: If your blood pressure remains high despite lifestyle changes, medications may be necessary. Certain drugs, like ACE inhibitors or ARBs, have been shown to protect both blood pressure and kidney function.
Final Thoughts
High blood pressure can be a silent killer, but it doesn’t have to silently destroy your kidneys. By understanding the impact of high blood pressure on your kidneys, being aware of the risk factors, and making a commitment to prevent them, you can save your kidneys and your quality of life. The answer to avoiding chronic kidney disease, dialysis, or a transplant is early detection and proactive management. Remember, your kidneys work tirelessly for you. Take action today to keep your kidneys strong and healthy.