[Research Report] The revenue cycle management market is expected to grow from US$ 98.34 billion in 2022 to US$ 244.64 billion by 2031; it is estimated to grow at a CAGR of 12.1% from 2022 to 2031.
Analyst Perspective:
The rise in government initiatives to encourage the use of revenue cycle management solutions is one of the major factors fueling the growth of the revenue cycle management market. Also, the rise in revenue loss from billing errors and process enhancements in healthcare institutions is boosting the growth of the revenue cycle management market. Correct handling of medical claims is essential to healthcare providers' revenue streams. Healthcare facilities must continue to maintain a high-quality insurance billing and revenue cycle in order to improve their financial result. The majority of healthcare providers are losing money as a result of claim denials and their failure to submit or postpone the denied claim, which is putting increasing pressure on hospitals to cut expenses. This has created an opportunity for the market players to come up with advanced solutions for hospitals to cater to the above challenges of the revenue cycle. Furthermore, for the efficient management of the revenue cycle, various key players in the market are integrating artificial intelligence (AI) and machine learning (ML) technologies, which will further propel the growth of the revenue cycle management market.
Market Overview:
Healthcare facilities utilize revenue cycle management (RCM), a financial process that tracks patient care episodes from registration and appointment scheduling to the last payment of a balance, using medical billing software. To store and manage patient billing records, healthcare providers frequently invest in revenue cycle management systems. When a patient progresses through the treatment process, an efficient RCM system can connect with other health IT systems, such as electronic health records (EHR) and medical billing systems, to shorten the time between performing a service and getting paid. Healthcare companies can also save time by automating tasks that employees previously performed with the help of an RCM system. Administrative tasks include notifying patients of forthcoming appointments, reminding payers and patients of outstanding balances, and contacting insurers with specific inquiries if a claim is rejected. RCM systems can also help providers save money by providing them with information about the reasons behind refused claims. This gives providers better insight into why some claims have been refused, allowing them to address the matter and preventing them from having to resubmit the claim.
Customize This Report To Suit Your Requirement
You will get customization on any report - free of charge - including parts of this report, or country-level analysis, Excel Data pack, as well as avail great offers and discounts for start-ups & universities
Revenue Cycle Management Market: Strategic Insights

- Get Top Key Market Trends of this report.This FREE sample will include data analysis, ranging from market trends to estimates and forecasts.
You will get customization on any report - free of charge - including parts of this report, or country-level analysis, Excel Data pack, as well as avail great offers and discounts for start-ups & universities
Revenue Cycle Management Market: Strategic Insights

- Get Top Key Market Trends of this report.This FREE sample will include data analysis, ranging from market trends to estimates and forecasts.
Market Driver:
Integration of AI and ML Technologies is Creating an Opportunity for the Growth of the Revenue Cycle Management Market
AI and ML technologies continue to gain momentum and prove their potential in the development of revenue management systems. Many organizations still rely on manual error checks and reports for anomaly detection, making it difficult to identify the root cause, and becoming a time-consuming process. ML and AI help organizations proactively identify anomalous patterns in billing and revenue management solutions. Further, the model continuously improves over time due to regular updates, which results in accurate billing and automation of detecting anomalies. AI and ML can also accelerate root cause analysis, reducing investigation time and costs and providing faster resolution using revenue management systems. Therefore, the growing technological advancements in billing and revenue management are likely to fuel the revenue cycle management market growth during the forecast period.
Segmental Analysis:
Based on components, the revenue cycle management market is segmented into solutions and services. The solutions segment held the largest share of the revenue cycle management market in 2022, whereas the service segment is estimated to register the highest CAGR in the revenue cycle management market during the forecast period. The RCM software is witnessing a rise in its adoption in the healthcare industry, particularly to avoid healthcare fraud and to decrease administrative costs. Furthermore, various key players in the market are continuously working on providing advanced solutions to improve revenue cycle management in hospitals, healthcare facilities, and others. Moreover, it is expected that due to the rise in the demand for cloud-based RCM and the increase in the demand for professional services, the service segment will grow with the highest CAGR in the revenue cycle management market.
Regional Analysis:
The healthcare industry in North America is changing quickly, and digitalization is making it easier to install healthcare IT services like revenue cycle management (RCM) systems, which use synchronized management software solutions to organize and streamline activities in healthcare businesses. Also, the growing focus of the healthcare sector on enhancing patient care while also taking advantage of the financial benefits and effectiveness of these cutting-edge, innovative RCM solutions provided by various market players in the region is fueling the growth of the market. In addition, the healthcare sector in the US is expanding and changing quickly due to several factors, including rising healthcare costs, an increase in the number of reputable healthcare facilities, rising healthcare IT spending, improving healthcare IT infrastructure, and a growing emphasis on the patient-provider relationship. Per the U.S. Centers for Medicare & Medicaid Services, National Health Expenditure (NHE) grew 2.7% to US$ 4.3 trillion in 2021 (US$ 12,914 per person) and accounted for 18.3% of GDP. Also, medicare spending grew 8.4% to US$ 900.8 billion in 2021, or 21% of total NHE. Medicaid spending grew 9.2% to US$ 734.0 billion in 2021, or 17% of total NHE. With such a rise in healthcare spending in the US, medical service providers are facing complex challenges in billing and precise payment, further raising the need for more advanced RCM systems.
Furthermore, various market players in the region are continuously working on providing advanced solutions. For instance, in 2023, the Healthcare Financial Management Association (HFMA) announced a strategic alliance with FinThrive, Inc., a healthcare revenue cycle management software-as-a-service (SaaS) provider, to co-launch a peer-reviewed, five-stage Revenue Cycle Management Technology Adoption Model (RCMTAM) designed to help health systems leverage industry benchmarks to assess their current state of RCM technology maturity and build best-practice plans to optimize revenue cycle outcomes. Thus, all the above factors are fueling the revenue cycle management market growth in North America.
Key Player Analysis:
Athenahealth Inc., Experian Information Solutions Inc., GE Healthcare, McKesson Corporation, NXGN Management LLC, Optum Inc., Oracle Corporation, R1 RCM Inc., The SSI Group, and Veradigm LLC are among the key revenue cycle management market players. These revenue cycle management market players are focused on continuous product development and innovation.
Recent Developments:
Inorganic and organic strategies such as mergers and acquisitions are highly adopted by companies in the revenue cycle management market. A few recent revenue cycle management market developments are listed below:
- In October 2023, Omega Healthcare announced the launch of its Omega Digital Platform (ODP), designed to help healthcare organizations reduce administrative burdens while improving financial performance. The ODP leverages advanced proprietary technologies to streamline workflows and improve financial performance. It utilizes deep domain and technology expertise in robotic process automation (RPA), AI & ML, bots, and natural language processing (NLP), which enables solutions to drive greater efficiency and accuracy.
- In June 2021, EXL, a leading operations management and analytics company, announced the launch of new Integrated Revenue Management Solutions from its EXL Health division. EXL Health has partnered with REVELOHEALTH, a provider of solutions dedicated to converting healthcare data into actionable information. EXL Health and REVELOHEALTH have combined their knowledge and expertise to provide new solutions that deliver a comprehensive, data-driven payment processing and revenue analytics capability. This new capability is structured to help providers optimize revenue cycle management, operating objectives, and compliance.
- In June 2021, Vee Technologies, a leading consulting and professional services organization, announced the launch of the Sona Suite of products and its flagship RCM workflow tool, Sona PROMISE. The RCM solution was designed to enhance operational workflows and enable business intelligence capabilities and is capable of being a standalone tool for managing hospitals, specialty practices, medical clinics, ambulatory surgery centers, and others. The solution was designed to simplify business operations and offer elevated business analytics for increased revenue and growth potential.
- In January 2021, R1 RCM Inc, a leading technology-enabled revenue cycle management (RCM) service provider for the healthcare sector, launched a new physician revenue cycle management solution, R1 Professional, for large independent practices and hospital-owned medical groups. The new solution is backed by a purpose-built technology platform, automation at scale, a digital patient financial experience aligned with consumer expectations, and proven performance improvement capabilities that empower financial visibility across large healthcare organizations.
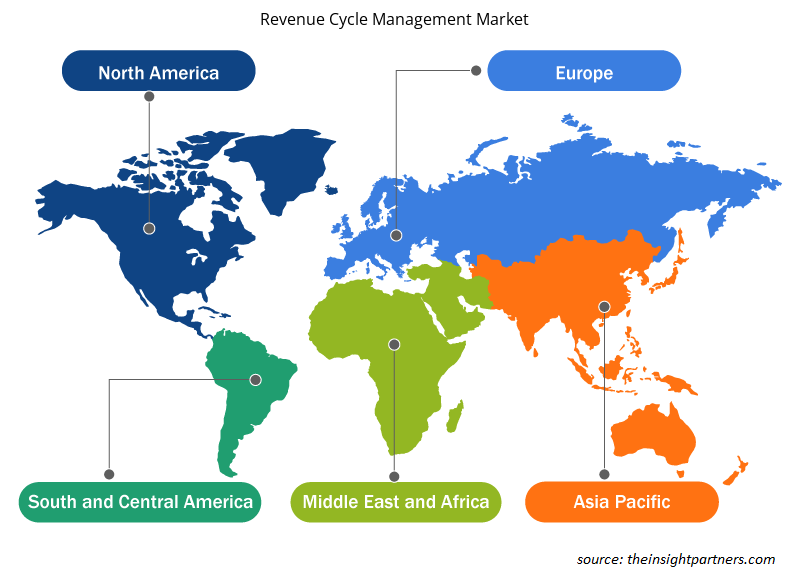
Revenue Cycle Management Market Regional Insights
The regional trends and factors influencing the Revenue Cycle Management Market throughout the forecast period have been thoroughly explained by the analysts at The Insight Partners. This section also discusses Revenue Cycle Management Market segments and geography across North America, Europe, Asia Pacific, Middle East and Africa, and South and Central America.
- Get the Regional Specific Data for Revenue Cycle Management Market
Revenue Cycle Management Market Report Scope
| Report Attribute | Details |
|---|---|
| Market size in 2024 | US$ XX million |
| Market Size by 2031 | US$ XX Million |
| Global CAGR (2025 - 2031) | 10.8% |
| Historical Data | 2021-2023 |
| Forecast period | 2025-2031 |
| Segments Covered |
By Component
|
| Regions and Countries Covered | North America
|
| Market leaders and key company profiles |
Revenue Cycle Management Market Players Density: Understanding Its Impact on Business Dynamics
The Revenue Cycle Management Market is growing rapidly, driven by increasing end-user demand due to factors such as evolving consumer preferences, technological advancements, and greater awareness of the product's benefits. As demand rises, businesses are expanding their offerings, innovating to meet consumer needs, and capitalizing on emerging trends, which further fuels market growth.
Market players density refers to the distribution of firms or companies operating within a particular market or industry. It indicates how many competitors (market players) are present in a given market space relative to its size or total market value.
Major Companies operating in the Revenue Cycle Management Market are:
- Allscripts Healthcare Solutions, Inc.
- Athenahealth, Inc.
- Cerner Corporation
- Eclinicalworks, LLC
- Epic Systems Corporation
Disclaimer: The companies listed above are not ranked in any particular order.

- Get the Revenue Cycle Management Market top key players overview
Frequently Asked Questions
What are the options available for the customization of this report?
Some of the customization options available based on request are additional 3-5 company profiles and country-specific analysis of 3-5 countries of your choice. Customizations are to be requested/discussed before making final order confirmation, as our team would review the same and check the feasibility.
What are the deliverable formats of Revenue Cycle Management Market report?
The report can be delivered in PDF/PPT format; we can also share excel dataset based on the request.
Which are the key players in the Revenue Cycle Management Market?
Key companies in this market are: Allscripts Healthcare Solutions Inc, Athenahealth Inc, Cerner Corporation, Eclinicalworks LLC, Epic Systems Corporation, Experian PLC, GE Healthcare, Gebbs Healthcare Solutions, McKesson Corporation
What is the expected CAGR of the Revenue Cycle Management Market?
The Revenue Cycle Management Market is expected to register a CAGR of 10.8% from 2023-2031.
What are the future trends in the Revenue Cycle Management Market?
Key future trends in this market are - Adoption of cloud-based solutions, Improved billing accuracy, Focus on cost reduction
What are the driving factors impacting the Revenue Cycle Management Market?
The major factors impacting the Revenue Cycle Management Market are: Shift Towards Value-Based Care, Increasing Regulatory Compliance Requirements, and Adoption of Advanced Technologies
- Historical Analysis (2 Years), Base Year, Forecast (7 Years) with CAGR
- PEST and SWOT Analysis
- Market Size Value / Volume - Global, Regional, Country
- Industry and Competitive Landscape
- Excel Dataset
- Parking Meter Apps Market
- eSIM Market
- Advanced Distributed Management System Market
- Online Exam Proctoring Market
- Electronic Data Interchange Market
- Barcode Software Market
- Maritime Analytics Market
- Cloud Manufacturing Execution System (MES) Market
- Robotic Process Automation Market
- Digital Signature Market
Testimonials
Reason to Buy
- Informed Decision-Making
- Understanding Market Dynamics
- Competitive Analysis
- Identifying Emerging Markets
- Customer Insights
- Market Forecasts
- Risk Mitigation
- Boosting Operational Efficiency
- Strategic Planning
- Investment Justification
- Tracking Industry Innovations
- Aligning with Regulatory Trends
Yes! We provide a free sample of the report, which includes Report Scope (Table of Contents), report structure, and selected insights to help you assess the value of the full report. Please click on the "Download Sample" button or contact us to receive your copy.
Absolutely — analyst assistance is part of the package. You can connect with our analyst post-purchase to clarify report insights, methodology or discuss how the findings apply to your business needs.
Once your order is successfully placed, you will receive a confirmation email along with your invoice.
• For published reports: You’ll receive access to the report within 4–6 working hours via a secured email sent to your email.
• For upcoming reports: Your order will be recorded as a pre-booking. Our team will share the estimated release date and keep you informed of any updates. As soon as the report is published, it will be delivered to your registered email.
We offer customization options to align the report with your specific objectives. Whether you need deeper insights into a particular region, industry segment, competitor analysis, or data cut, our research team can tailor the report accordingly. Please share your requirements with us, and we’ll be happy to provide a customized proposal or scope.
The report is available in either PDF format or as an Excel dataset, depending on the license you choose.
The PDF version provides the full analysis and visuals in a ready-to-read format. The Excel dataset includes all underlying data tables for easy manipulation and further analysis.
Please review the license options at checkout or contact us to confirm which formats are included with your purchase.
Our payment process is fully secure and PCI-DSS compliant.
We use trusted and encrypted payment gateways to ensure that all transactions are protected with industry-standard SSL encryption. Your payment details are never stored on our servers and are handled securely by certified third-party processors.
You can make your purchase with confidence, knowing your personal and financial information is safe with us.
Yes, we do offer special pricing for bulk purchases.
If you're interested in purchasing multiple reports, we’re happy to provide a customized bundle offer or volume-based discount tailored to your needs. Please contact our sales team with the list of reports you’re considering, and we’ll share a personalized quote.
Yes, absolutely.
Our team is available to help you make an informed decision. Whether you have questions about the report’s scope, methodology, customization options, or which license suits you best, we’re here to assist. Please reach out to us at sales@theinsightpartners.com, and one of our representatives will get in touch promptly.
Yes, a billing invoice will be automatically generated and sent to your registered email upon successful completion of your purchase.
If you need the invoice in a specific format or require additional details (such as company name, GST, or VAT information), feel free to contact us, and we’ll be happy to assist.
Yes, certainly.
If you encounter any difficulties accessing or receiving your report, our support team is ready to assist you. Simply reach out to us via email or live chat with your order information, and we’ll ensure the issue is resolved quickly so you can access your report without interruption.











The List of Companies
1. Allscripts Healthcare Solutions, Inc.
2. Athenahealth, Inc.
3. Cerner Corporation
4. Eclinicalworks, LLC
5. Epic Systems Corporation
6. Experian PLC
7. GE Healthcare
8. Gebbs Healthcare Solutions
9. Mckesson Corporation
10. Quest Diagnostics Incorporated






 Get Free Sample For
Get Free Sample For